This issue brief is the first of a two-part series examining the behavioral health workforce shortage in Kansas. It focuses on the types, training, licensure and quantity of certain behavioral health providers in the state. The second brief in the series, Addressing Behavioral Health Workforce Needs in Kansas, describes the age and geographic distribution of a large segment of the Kansas behavioral health workforce, as well as strategies to reduce the workforce shortage. An earlier series of issue briefs examined the primary care workforce shortage and the age and geographic distribution of primary care physicians in Kansas.
Defining the Behavioral Health Workforce in Kansas
9 Min Read
Dec 20, 2022
By
Cynthia Snyder, M.A., Angela S Wu, M.S.,Hina B. Shah, M.P.H.,
Wen-Chieh Lin, Ph.D.
Key Points
- Behavioral health providers are a diverse group of professionals who treat mental health conditions and substance use disorders.
- There were approximately 440 prescribing psychiatric clinicians physically located and practicing in Kansas in 2021, including 300 psychiatrists, 23 physician assistants and 117 advance practice registered nurses.
- There were 2,414 non-prescribing, top-level independent practice behavioral health clinicians physically located and practicing in Kansas in 2021, including 314 licensed psychologists, 1,141 licensed specialist clinical social workers, 322 licensed clinical addiction counselors, 323 licensed clinical marriage and family therapists and 314 licensed clinical professional counselors.
- Primary care providers also may address mental health and substance use disorders in their practices, especially in rural areas.
Introduction
In many behavioral health professions, the workforce supply does not meet community demand, and projections for the future indicate increasing challenges. The Health Resources and Services Administration (HRSA) estimates by 2025 there will be a 1 percent reduction in psychiatrists and social workers addressing mental health and substance use disorders nationwide, contrasted with an increased demand for psychiatrists of 6 percent and social workers of 14 percent, compared to 2013. In addition to the forces driving national trends, Kansas has long-standing workforce shortages, access issues from distribution of the workforce across the state, and an aging workforce. Out of 105 Kansas counties, 99 are designated as Mental Health Professional Shortage Areas based on the availability of psychiatrists to meet the needs of the population. The Kaiser Family Foundation estimates that Kansas would need an additional 64 psychiatrists to remove the current shortage designations.
Behavioral Health Workforce
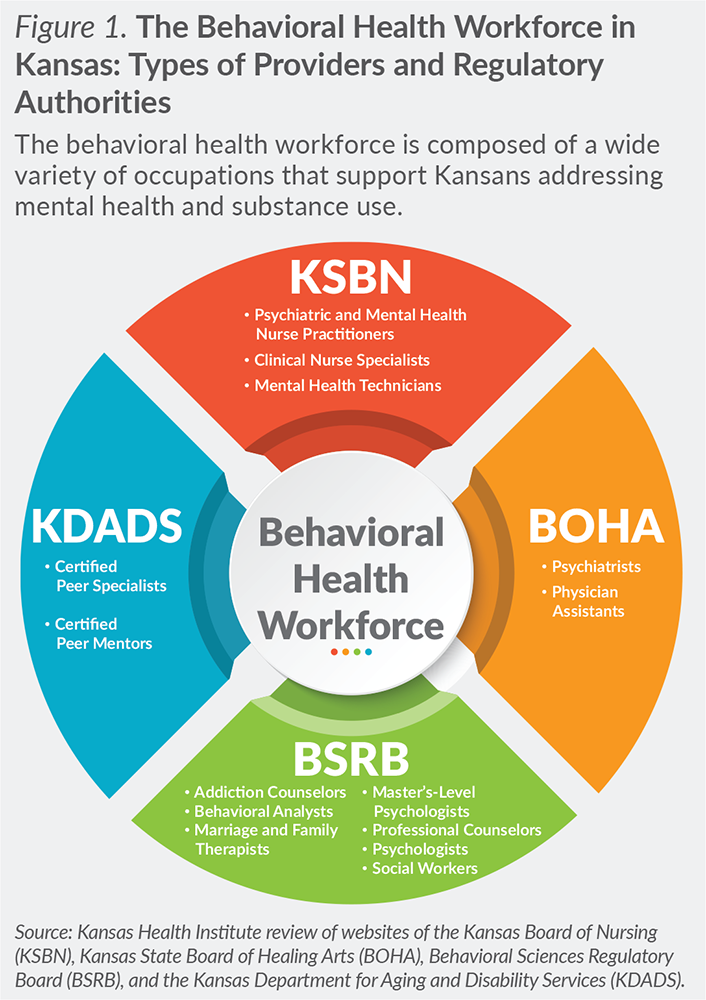
In Kansas, the behavioral health workforce is built on a complex landscape of regulators, fields of practice, and license levels within each field. As shown in Figure 1, the Kansas State Board of Healing Arts (BOHA) regulates psychiatrists and physician assistants (PA); the Kansas Board of Nursing (KSBN) regulates psychiatric and mental health nurse practioners, clinical nurse specialists and mental health technicians; the Kansas Behavioral Sciences Regulatory Board (BSRB) regulates seven behavioral health fields including addiction counselors, behavior analysts, marriage and family therapists, master’s level psychologists, professional counselors, psychologists and social workers; and the Kansas Department for Aging and Disability Services (KDADS) regulates certified peer specialists and certified peer mentors. Community Health Workers have not been regulated, but the Kansas Department of Health and Environment has recently established a certification program.
Also, within this complex landscape of behavioral health care, there are both prescribers and non-prescribers, as well as fields that focus on mental health and those that focus specifically on addictions and substance use disorders. This brief focuses on independent practice clinicians.
Prescriber Behavioral Health Workforce
Psychiatrists, psychiatric APRNs and psychiatric PAs are able to prescribe and monitor medications, as well as diagnose and treat behavioral health conditions. Medications can play an important role in treating mental health and substance use disorders, in addition to talk therapy and other treatment modalities. An adequate prescriber workforce is needed to address medical and complex psychological issues and to monitor the effectiveness and side effects of medications. Altogether, there were approximately 440 prescribing psychiatric clinicians in Kansas in 2021.
Kansas has 300 psychiatrists that are physically located in Kansas and practice outpatient behavioral health. Kansas has an additional 81 psychiatrists registered with BOHA, but practicing in academic, research, inpatient hospital and correctional settings, providing telehealth from out-of-state only, or no longer practicing in Kansas. This analysis does not include practitioners from neighboring states without a Kansas business address on their license application. Kansas has a long-standing shortage of psychiatrists and limited capacity to add the estimated 64 additional psychiatrists needed to eliminate shortage areas. In addition to the increase in the total workforce needed, Kansas also will have to replace an aging workforce as described in the second brief in this series, Addressing Behavioral Health Workforce Needs in Kansas.
APRNs specializing in psychiatry or mental health comprise a small proportion of the prescriber workforce (26.6 percent). There are 21 psychiatric clinical nurse specialists and 96 psychiatric nurse practitioners licensed with KSBN. Because PA specialty information was not available in the licensure data, the number of psychiatric PAs is estimated using the proportion of PAs practicing psychiatry, the smallest certified practice area, published by the National Commission on Certification of Physician Assistants (NCCPA). According to the NCCPA, 1.8 percent of PAs were practicing behavioral health in 2020. The estimate for Kansas is 23 PAs working under the supervision of a psychiatrist. Growth in both fields is an opportunity to meet the increased demand and address mental health workforce shortages.
Non-Prescriber Behavioral Health Workforce
Non-prescribers also address the diagnosis and treatment of behavioral health disorders, often working in conjunction with the prescribing workforce. The non-prescribing workforce, depending on specialty and license, offers a range of services including peer support, case management, talk therapy and other treatment modalities.
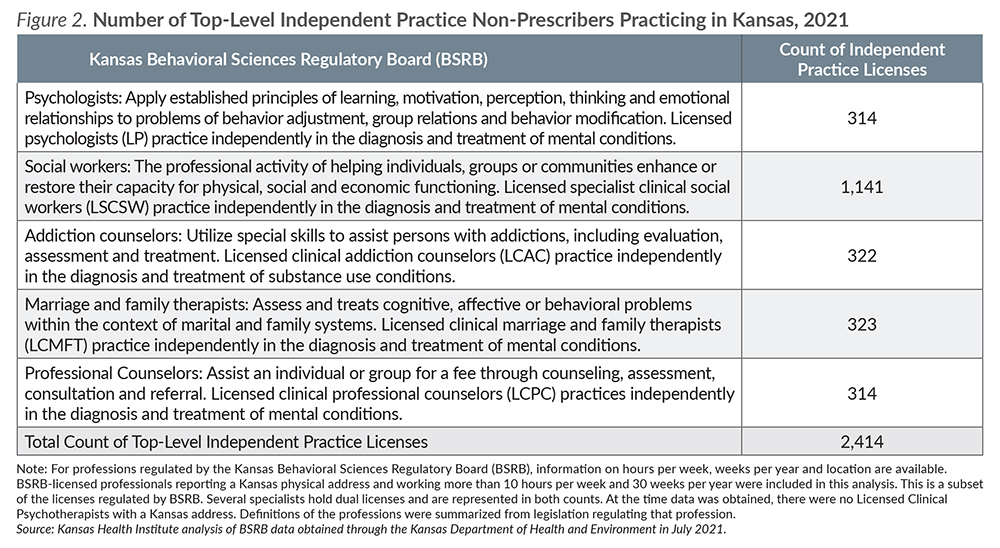
BSRB regulates most of the non-prescriber workforce. The independent practice level of five fields is outlined in Figure 2, highlighting the large number of licensed specialist clinical social workers (LSCSW) in the workforce. LSCSWs outnumber 3 to 1 any of the other independent practice behavioral health specialties. There are 1,141 LSCSWs compared to a total of 1,273 of all other independent practice behavioral health professionals. This analysis does not include clinicians without a Kansas business address on their license applications. Unlike psychiatrists, estimates of workforce shortages in the non-prescriber workforce are not monitored. Among these professionals, the adequacy of supply and demand will need to be assessed to determine workforce needs.
Several specialists regulated by BSRB hold more than one license to extend training and scope of practice in more than one area. The most common dual license among LSCSWs is the licensed clinical addition counselor (LCAC), an independent practice license specializing in addiction. There are 133 specialists who hold both licenses in Kansas, representing about a tenth (11.7 percent) of the LSCSW workforce.
Training and Supervision Requirements
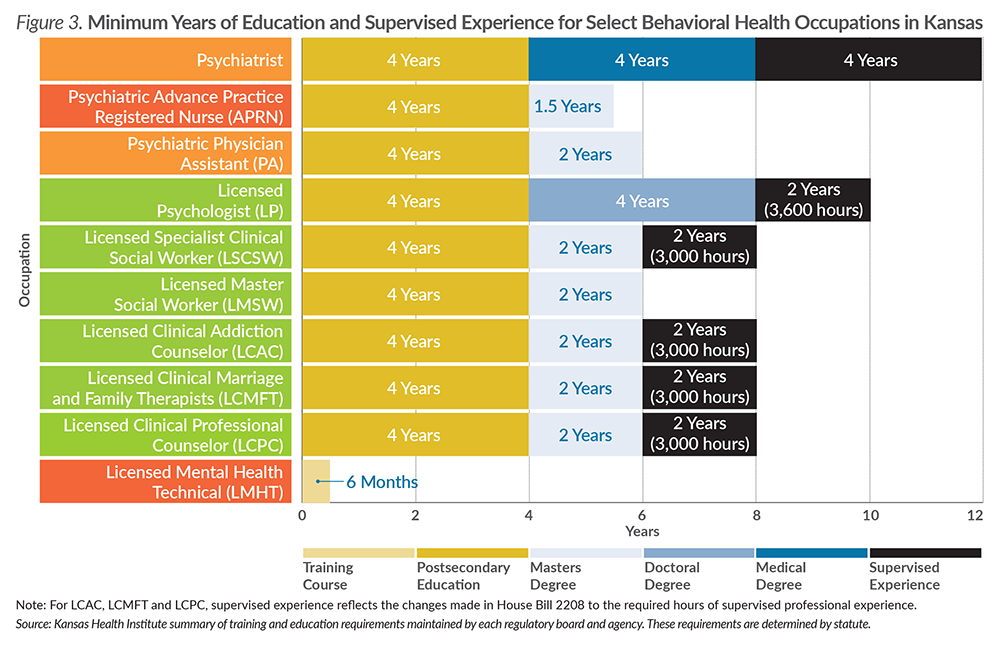
The education and supervision requirements (Figure 3) of the range of behavioral health professionals illustrate two key steps in the behavioral health workforce pipeline. To achieve independent practice and the top-level license in their respective fields, non-prescribing behavioral health professionals must often complete a master’s degree and a minimum of two years of supervised professional experience. Legislation enacted in 2021 addressed increasing health care capacity, including reducing the minimum supervised professional experience from 4,000 hours to 3,000 hours for many top-level licenses from BSRB. The changes also reduced the minimum direct client contact hours and face-to-face supervision requirements. These changes reduce some of the burden in supplying the behavioral health workforce, but other barriers remain.
Ability to Independently Practice
Within each of the professions regulated by BSRB, there are various licenses reflecting different levels of education, training and expertise. Social workers, for example, include bachelor’s and master’s levels with independent practice at the licensed specialist clinical social worker (LSCSW) level. However, LSCSWs are not the largest group of license holders. There are 1,443 licensed master social workers (LMSW) working at least 10 hours a week and 30 weeks a year as social workers, representing a large potential pool for the independent practice workforce. LMSWs and LSCSWs have the same minimum education standards. However, LSCSWs have met the additional requirements of licensure, including post-graduate supervision, thus granting them independent practice and additional payment models. LMSWs have limited placement and payment options, despite the need to complete 3,000 hours of professional experience to become LSCSWs.
Behavioral Health Services in a Medical Primary Care Setting
Primary care providers (PCP) also provide behavioral health services within their medical practices. PCPs see the consequences of behavioral health conditions on physical illness, mortality, treatment outcomes and higher health care costs. Behavioral health in a primary care medical setting can range from prescribing and monitoring medication to a fully integrated care model with on-site behavioral health staff included in the treatment team.
The National Center for Health Statistics (NCHS) estimated that there were 30 million mental health-related office visits annually between 2012-2014 with physicians. Over one-half (55 percent) of the mental health related visits were with a psychiatrist, one-third (32 percent) were with a primary care physician and the remainder were with other specialists (13 percent). The analysis was based on the primary reason for the visit and does not include behavioral health issues listed as secondary or tertiary reasons, or identified during intake screening, which would increase the proportion of visits with a PCP.
The NCHS study also shows that, in urban areas, 6 in 10 (63 percent) mental health office visits were with a psychiatrist, as compared to one-quarter (26 percent) with a primary care physician. In rural areas, the pattern was reversed with 3 in 10 (29 percent) visits with psychiatrists and slightly more than one-half (54 percent) with primary care providers. As outlined in the second brief, there are significant differences in the urban/rural distribution of psychiatrists in Kansas that may make that contrast even more vivid.
PCPs make a significant contribution to addressing mental health and substance use disorders, especially in rural areas. In Kansas, there are 300 psychiatrists, as compared to 1,976 PCPs. In addition, with integrated care, PCPs can work in coordination with behavioral health providers to provide access to services and improve outcomes.
About Kansas Health Institute
The Kansas Health Institute supports effective policymaking through nonpartisan research, education and engagement. KHI believes evidence-based information, objective analysis and civil dialogue enable policy leaders to be champions for a healthier Kansas. Established in 1995 with a multiyear grant from the Kansas Health Foundation, KHI is a nonprofit, nonpartisan educational organization based in Topeka.