Direct to consumer telemedicine, which is a common form of telehealth, involves real-time communication between a patient and a provider via telephone or videoconference. Direct to consumer telemedicine has been used for a variety of conditions and services and is often provided by companies such as Teledoc, American Well and Doctor on Demand.
Utilization
Use of telehealth prior to the pandemic was low — but increasing — as seen in both the number of individuals receiving telehealth as well as the volume of services provided via telehealth.
Among 22 states with telemedicine reimbursement for Medicaid in 2008-2009, only 0.1 percent of enrollees received services via telemedicine. Similarly, a study that included patients with public or private insurance found that only 0.7 percent of patients received telemedicine services between 2010 and 2015, although the rate of telehealth users per 10,000 enrollees increased during the study period.
In the Texas Medicaid program, the number of clients using telehealth, telemedicine and home telemonitoring increased by 30 percent from fiscal year (FY) 2016 to FY 2017, and the percentage of veterans using clinical video telemedicine (CVT) in the Veterans Health Administration (VHA) increased from 1.2 percent to 4.6 percent from FY 2009 to FY 2015.
The volume of services provided via telehealth was also growing prior to the pandemic. In Minnesota, telemedicine visits grew by 600 percent from 2010 to 2015, and CVT encounters grew 421 percent in the VHA from FY 2009 to FY 2015.
Rural Populations
Telehealth has been touted by many as one option to increase access to services for individuals living in rural areas.
Prior to COVID-19, telehealth services provided to rural residents were more likely to be covered by public health insurance. Among Minnesota telemedicine users in nonmetropolitan areas in 2015, more than 60 percent were covered by public insurance such as Medicaid, Medicare or both. Among telemedicine users in metropolitan areas, only 20 percent were covered by public health insurance.
Among Medicaid telemedicine patients in 22 states where those services were reimbursed, those living in rural areas were 17 times more likely to receive telemedicine care than their metropolitan counterparts. In another study, VHA patients living in rural areas or at a greater distance to a VHA facility were more likely to use CVT and the rate of utilization grew more quickly among rural patients.
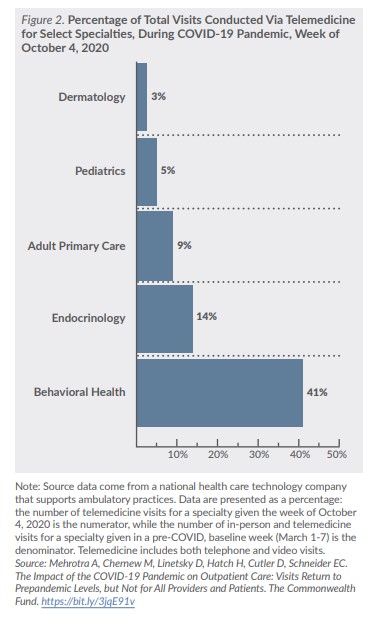
Behavioral Health Care
While telehealth has been used to deliver a variety of health services, behavioral health services, including mental health and substance use disorder (SUD) services, are among the most common. Among VHA patients, at least half of all CVT encounters in FY 2009 and FY 2015 were for mental health care, although use of telemedicine for other specialties grew during the study period. Among Medicaid patients in 22 states with telemedicine reimbursement in 2008-2009, nearly 93 percent of telemedicine claims were associated with a behavioral health diagnosis. In Minnesota, while only about one-third of telemedicine services in 2015 were provided by physicians, the majority (51.5 percent) of those physicians were psychiatrists.
Higher utilization of telehealth for behavioral health services compared to other specialties could be due to many factors, including earlier adoption of telehealth by behavioral health providers, ease of delivering behavioral health care virtually compared to other disciplines (e.g., it does not require a physical exam) and regulatory differences across states.